In 2021, microbiologist Adwoa Padiki Nartey caught a bacterial infection and her tonsils started to swell. She’d had the same symptoms the year before; both illnesses occurred during one of two annual rainy seasons in Ghana’s capital, Accra, where she lives. In these seasons, she knew, high humidity and moisture spur microbial growth. Doctors prescribed antibiotics but, unlike before, the drugs didn’t work. The bacteria had become resistant.
Over two weeks, her tonsils became increasingly inflamed. “It was painful to drink. Painful to eat. I could barely speak,” says Padiki Nartey, who researches antibiotic resistance at the University of Ghana in Accra. “I was worried.”
To her relief, a final combination of two types of antibiotic worked. Otherwise, the infection could have killed her, she says. “That’s pretty scary.”
The fight against antimicrobial resistance
The episode demonstrates how two major threats to human health — climate change and the spread of antibiotic resistance — can intersect. Climate change has led to more frequent heavy rainfall in Ghana, Padiki Nartey says. Those conditions, in turn, encourage bacterial growth, including that of antibiotic-resistant microbes. Flooding also spreads antibiotic-resistant bacteria from sewage systems into people’s homes and drinking water, she adds.
Although researchers have some understanding of how climate change will exacerbate the rise in antibiotic resistance, scientists are now digging into the mechanisms and exploring how large the effect could be, says Pamela Yeh, an evolutionary biologist at the University of California, Los Angeles. “Climate change and antibiotic resistance are two of the biggest health issues of our time,” she says. “Researchers are starting to look at how they link up.”
Climbing resistance
Drug-dodging bacteria are on the rise. In 2020, human blood infections caused by antibiotic-resistant Neisseria gonorrhoea, Escherichia coli and Salmonella bacteria became at least 15% more common than in 2017, according to a report published by the World Health Organization (WHO) in 2022. We are hurtling towards a world where scraping your knee, giving birth or having a simple surgical procedure could kill you, says Yeh. “It’s incredibly frightening,” she says.
The key problem is that antibiotics are often overused or misused to fight infections in people, other animals and plants. Bacteria can develop resistance to drugs through DNA mutations that alter the bacterial cell wall such that antibiotics can’t work, or that confer abilities to break down antibiotics or pump them out of cells. Strains that become resistant can also share antibiotic-resistance genes with other bacteria. If the wrong antibiotics are given to treat infections, or if the right drugs are taken at insufficient doses to kill the microorganisms, then the microbes have more time to multiply and to evolve or spread resistance.
But as in Ghana, changing weather conditions that help bacteria thrive also play a part. And disasters stemming from extreme weather events such as floods, droughts, hurricanes and wildfires can exacerbate the issue because they often reduce access to clean water, leading to unsanitary conditions. When injuries and infections start to rise, more people use antibiotics, in turn pushing up the likelihood of resistance developing.
In a study1 published last October, microbiologist Rita Colwell at the University of Maryland in College Park and her colleagues showed that a deadly hurricane had led to a spike in harmful species of antibiotic-resistant Vibrio bacteria — including a flesh-eating species — in waters off the coast of Florida. The high winds whipped up nutrients from marine sediments that the bacteria thrive on, says Colwell.
Temperature changes
Beyond the physical damage caused by extreme weather, researchers are exploring how rising temperatures that result from climate change might influence antibiotic resistance. In November 2022, microbiologist Lianping Yang at Sun Yat-sen University in Guangzhou, China, and his colleagues reported on the prevalence of three bacteria behind antibiotic-resistant hospital infections that are often severe and can be deadly: Acinetobacter baumannii, Klebsiella pneumoniae and Pseudomonas aeruginosa2.
The researchers looked for links between temperature and antibiotic resistance by comparing bacterial data — collected from people treated in hospitals in 28 provinces and regions across China — with information on average air temperatures in cities in the same regions. The team corrected for factors that could affect rates of drug resistance, including the level of antibiotic consumption, average humidity, yearly rainfall and population density.
They found that, for every 1 °C increase in average air temperature, there was a 14% increase in the proportion of samples containing K. pneumoniae that were resistant to a type of antibiotic called carbapenems. These drugs are usually reserved for treating bacteria that are resistant to all other antibiotics.
Yang and his colleagues also linked a 1 °C increase in average air temperature to a 6% increase in the proportion of samples containing carbapenem-resistant P. aeruginosa. But temperature did not significantly affect the prevalence of drug-resistant A. baumannii.
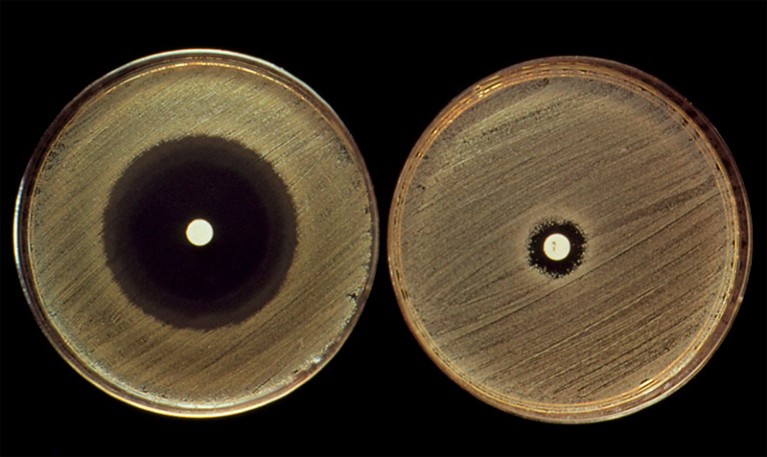
Widely used antibiotics such as penicillin (in white spots) can have very different effects on related bacterial strains (opaque growths).Credit: John Durham/SPL
These findings support studies from 2018 and 2020 by microbiologist Derek MacFadden at the University of Ottawa and his colleagues3,4. The team found that increased average minimum temperatures were linked to higher rates of antibiotic resistance across 41 states in the United States3 and 28 countries in Europe4. However, the studies do not show a causal link between temperature and antibiotic resistance, says Yang.
One way that gradual increases in average air temperature could be driving up antibiotic resistance is by increasing the growth rate of bacteria, speeding up their evolution, says MacFadden. There is also evidence that bacteria can share genes — including elements that confer antibiotic resistance — more easily in warm conditions than in cold ones5.
Extreme conditions
Another idea is that very high temperatures — which are experienced more often as the globe warms, even though average temperatures rise only slightly — might induce genetic changes in bacteria that help them to resist antibiotics, says Yang.
In a 2018 study, Yeh and her colleagues exposed E. coli, which grew best at 41 °C, either to a temperature of 44 °C or to a range of 12 antibiotics (deliberately given at low doses to inhibit but not kill all the bacteria)6. The researchers tracked how the bacteria responded to these stressors, and found that patterns of gene expression changed in similar ways for both temperature and antibiotic type. In both cases, bacteria responded to the stress by producing more ‘heat-shock’ proteins. These help other proteins to fold correctly and apparently also help bacteria to survive antibiotic attack, says Yeh. “We sometimes call antibiotics that mimic [the effects of] hot conditions ‘hot’ drugs,” she says.
When E. coli was exposed to temperatures as low as 22 °C, the microbes ramped up ‘cold-shock’ proteins — again helping them to produce the proteins needed for survival. Some ‘cold’ antibiotics, such as tetracycline, altered bacterial gene activity in a similar way.
COP28 climate summit signals the end of fossil fuels — but is it enough?
The findings suggest that bacteria that have evolved in extremely hot or cold conditions might be more resistant to certain antibiotics, Yeh says. But in a study that is yet to be published, Yeh’s team found that exposure to high temperatures sometimes makes bacteria less resistant to ‘hot’ antibiotics, highlighting that the links between temperature and resistance are likely to be complex, she says.
Extreme temperatures could also contribute to antibiotic resistance by changing how people interact with each other, says MacFadden.
In South Korea, “when we reach the highest temperatures, people tend to stay inside”, says microbiologist Soojin Jang at the Pasteur Institute Korea in Seongnam. Bacteria tend to spread particularly easily between people who are in close contact with each other indoors, she says. That could help to spread resistant strains, and — because more bacteria are multiplying in more people — increase the chance that resistance will emerge.
Over the past year, Jang and her team have been tracking the presence of antibiotic-resistance genes in bacterial samples collected from public toilets, trains and buses. The researchers hope to continue this over the next decade and compare rates of antibiotic resistance with factors such as local air temperature and social behaviour. This could help to reveal how climate change is affecting the spread of resistance, says Jang.
Tackling resistance
Surveillance such as Jang’s could be allied with climate and weather data to help track or predict the spread of antibiotic-resistant bacteria, says Colwell. In a study published last February, she and her colleagues used factors including temperature and rainfall data from satellites to predict when and where cholera outbreaks — caused by the waterborne bacteria Vibrio cholerae — would occur7. Their machine-learning model predicted the risk of cholera outbreaks in various regions across Yemen with an average accuracy of 72%, and up to four weeks in advance.
Combining weather data with surveillance for antibiotic-resistance genes by monitoring waste water could improve forecasts for areas that are at a high risk of antibiotic resistance, Colwell says. It’s an approach her team is working on.

Hurricane Ian caused flooding in the streets of Fort Myers, Florida, in 2022.Credit: Pedro Portal/Miami Herald/Tribune News Service via Getty
Besides improving surveillance, researchers already know what’s needed to reduce the spread of antibiotic-resistant bacteria: improving access to clean water and sanitary facilities, and raising awareness of how to use antibiotics appropriately.
Some efforts have been successful. In Lebanon, for instance, clinician and infectious-disease researcher Souha Kanj says a programme that she and her colleagues started at the American University of Beirut in 2018 educated physicians on how to reduce the use of carbapanem antibiotics in their hospital. In 2020, the proportion of A. baumannii infections that were carbapenem-resistant had fallen to 63%, from 81% at the start of the programme8.
Padiki Nartey, meanwhile, is among those trying to develop new ways to kill drug-resistant bacteria. One particularly promising approach is to use viruses called phages, which infect bacteria, but not human cells.
Global action
Researchers seeking to stem the rise of antibiotic resistance could also learn lessons from climate-change politics, says Steven Hoffman, an international lawyer and health-policy researcher at York University in Toronto, who is also at the Public Health Agency of Canada. Such global threats don’t respect national borders, says microbiologist Saffiatou Darboe at the University of the Gambia in Serrekunda. So, drawing parallels with climate change, countries should agree a global treaty to tackle the issue, Hoffman says.
In 2015, the WHO launched a Global Antimicrobial Resistance and Use Surveillance System (GLASS), which helps to track the global consumption of antibiotics and the prevalence of common antibiotic-resistant infections. These data are used as an indicator in the United Nations Sustainable Development Goals to monitor progress on tackling antimicrobial resistance.
The world’s goals to save humanity are hugely ambitious — but they are still the best option
But stronger action is needed, says Hoffman. In a 2022 study9, he and his colleagues called for a treaty to tackle drug-resistant pathogens — equivalent to the 2015 Paris climate agreement. He wants countries to articulate a single unifying goal, such as a 35% reduction in drug-resistant infections by 2035, and hopes that they will make progress on this when they convene at a UN meeting on antimicrobial resistance in September. The meeting is only the second time that the issue has been the subject of a UN General Assembly.
And just as richer nations have agreed to pay poorer ones to help deal with the effects of climate change, so they should financially support poorer nations facing a higher prevalence of antibiotic resistance, Hoffman adds. “Richer countries have benefited for much longer from antimicrobials,” he says.