In a world first, the UK medicines regulator has approved a therapy that uses CRISPR gene editing as a treatment for diseases. The decision marks another high point for a biotechnology that has regularly been lauded as revolutionary in the decade since its discovery.
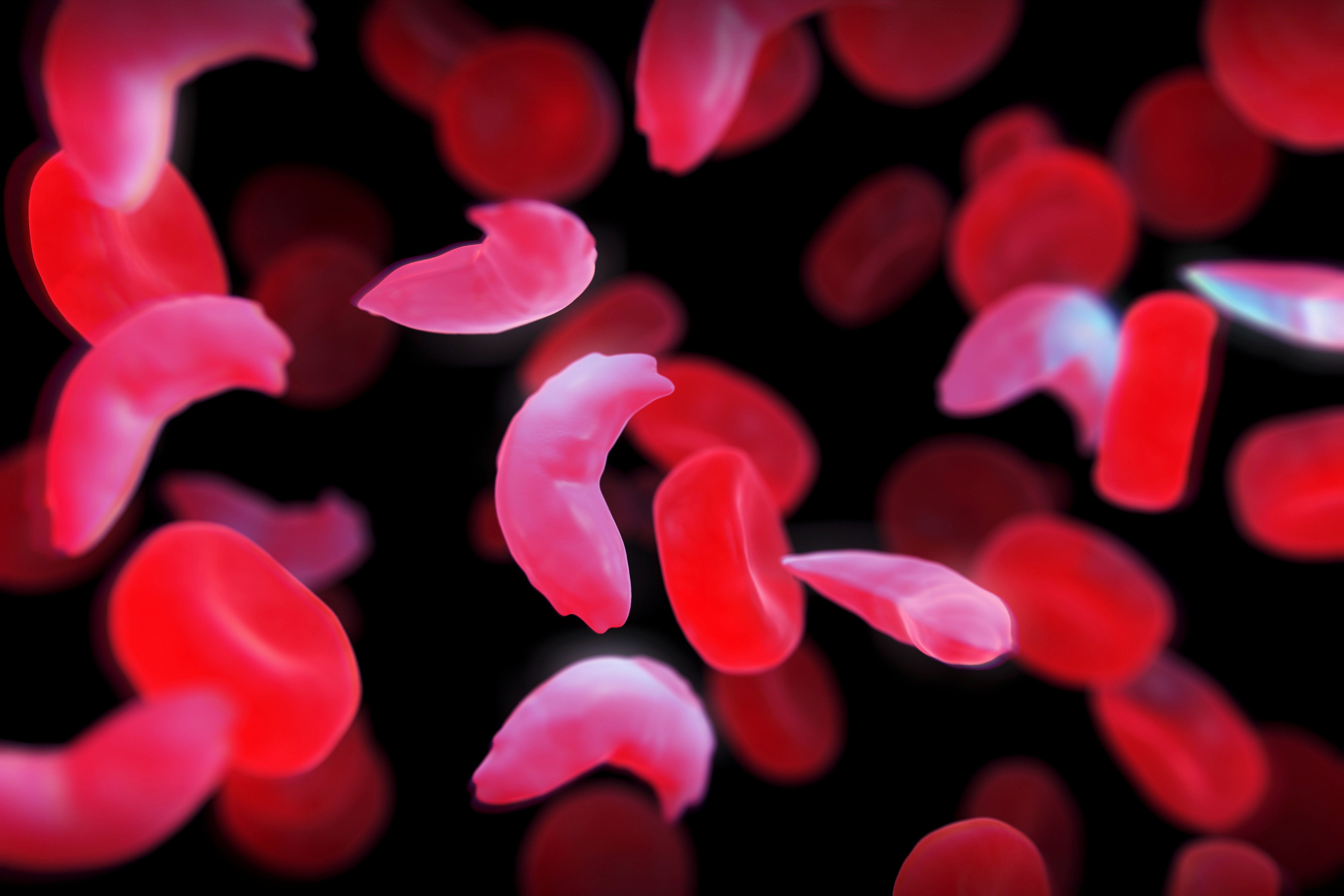
The therapy, called Casgevy, will treat the the blood conditions sickle-cell disease and β-thalassaemia. Sickle-cell disease, also known as sickle-cell anaemia, can cause debilitating pain, and people with β-thalassaemia can require regular blood transfusions.
“This is a landmark approval which opens the door for further applications of CRISPR therapies in the future for the potential cure of many genetic diseases,” said Kay Davies, a geneticist at the University of Oxford, UK, in comments to the UK Science Media Centre.
Nature explains the research behind the treatment and explores what’s next.
What research led to the approval?
The approval by the Medicines and Healthcare products Regulatory Agency (MHRA) follows promising results from clinical trials that tested the one-time treatment, which is administered by intravenous infusion and was developed by Vertex Pharmaceuticals in Boston, Massachusetts, and CRISPR Therapeutics in Zug, Switzerland.
The trial for sickle-cell disease has followed 29 out of 45 participants long enough to draw interim results. Casgevy completely relieved 28 of those people of debilitating episodes of pain for at least one year after treatment.
Researchers also tested the treatment for a severe form of β-thalassaemia, which is conventionally treated with blood transfusions roughly once a month. In this trial, 54 participants received Casgevy and 42 patients have participated for long enough to provide interim results. For at least one year after treatment, 39 participants, or 93% of those treated, did not need a red-blood-cell transfusion. The remaining three people had their need for blood transfusions reduced by more than a 70%.
How does the gene therapy work?
Casgevy relies on the gene-editing tool CRISPR, the developers of which won the Nobel Prize in Chemistry in 2020.
Sickle-cell disease and β-thalassaemia are caused by errors in the DNA sequence of genes that encode for haemoglobin, a molecule that helps red blood cells to carry oxygen around the body.
In sickle-cell disease, abnormal haemoglobin makes blood cells misshapen and sticky, causing them to form clumps that can clog blood vessels. These blockages reduce the oxygen supply to tissues, which can cause periods of severe pain, known as pain crises.
β-thalassaemia occurs when mutations in the haemoglobin gene lead to deficient or absent levels of the oxygen-carrying molecule in red blood cells, low numbers of red blood cells and symptoms such as fatigue, shortness of breath and irregular heartbeats.
Clinicians administer Casgevy by taking blood-producing stem cells out of the bone marrow of people with either disease and using CRISPR to edit genes encoding for haemoglobin in these cells. The gene-editing tool an RNA molecule that guides the enzyme to the correct region of DNA and a Cas9 enzyme that cuts DNA.
Once the Cas9 enzyme reaches the gene targeted by Casgevy, called BCL11A, it cuts both DNA strands. BCL11A usually prevents the production of a form of haemoglobin that is made only in fetuses. By disrupting the BCL11A gene, Casgevy unleashes the production of fetal haemoglobin, which does not carry the same abnormalities as adult haemoglobin in people with sickle cell or β-thalassaemia patients.
Before the gene-edited cells are infused back into the body, people must undergo a treatment that prepares the bone marrow to receive the edited cells. Once administered, the stem cells give rise to red blood cells containing fetal haemoglobin. After some time, this relieves symptoms by boosting the oxygen supply to tissues. “Patients may need to spend at least a month in a hospital facility while the treated cells take up residence in the bone marrow and start to make red blood cells with the stable form of haemoglobin,” the MHRA said in a press release.
How safe is Casgevy?
Participants involved in the trials, which are ongoing, experienced side effects including nausea, fatigue, fever and an increased risk of infection, but no significant safety concerns were identified. The MHRA and manufacturer are monitoring the safety of the technology and will release further results.
One concern surrounding the approach is that CRISPR can sometimes make unintended genetic modifications with unknown side effects.
“It is well known that CRISPR can result in spurious genetic modifications with unknown consequences to the treated cells,” geneticist David Rueda at Imperial College London told the SMC. “It would be essential to see the whole-genome sequencing data for these cells before coming to a conclusion. Nonetheless, this announcement makes me feel cautiously optimistic.”
Will other countries approve the treatments?
The US Food and Drug Administration is considering approval of Casgevy, whose generic name is exa-cel, for sickle-cell disease; its advisers met last month to discuss the therapy. The European Medicines Agency is also reviewing the treatment for both diseases.
For now, the therapy is likely to remain the reserve of rich nations with developed health-care systems. “This treatment may not easily scale up to be able to provide treatments in low- and middle-income countries, since it requires the technology to obtain a patient’s blood stem cells, deliver the genetic editor to these stem cells, and then reinjection of these cells,” geneticist Simon Waddington at University College London told the SMC. “It is not an ‘off the shelf’ medicine that can be readily injected or taken in pill form,” he says.
How much will it cost?
Even in places where it win approval, the high cost of Casgevy is likely to limit who can benefit from it.
“The challenge is that these therapies will be very expensive so a way of making these more accessible globally is key,” said Davies.
The treatment’s price has not yet been settled in the United Kingdom, but estimates suggest that it could cost roughly US$2 million per patient, in line with the pricing of other gene therapies.
“We have not established a list price for the UK at this time and are focused on working with the health authorities to secure reimbursement and access for eligible patients as quickly as possible,” a Vertex spokesperson told Nature.
This article is reproduced with permission and was first published on November 16, 2023.